Tonix is committed to developing therapeutics that improve the lives of patients suffering from chronic, often overlooked conditions, with a focus on central nervous system (CNS) disorders. Relying on in-house discovery as well as external collaborations, Tonix has transformed into a company that now includes biologic product candidates, in addition to small molecule drug candidates, targeting an array of CNS disorders.
Fibromyalgia
Fibromyalgia (FM) is a chronic pain disorder that is understood to result from amplified sensory and pain signaling within the central nervous system. FM afflicts an estimated 6-12 million adults in the U.S.1, approximately 90% of whom are women. Symptoms include chronic widespread pain, nonrestorative sleep, fatigue, and morning stiffness. Other associated symptoms include cognitive dysfunction and mood disturbances, including anxiety and depression. Individuals suffering from fibromyalgia struggle with their daily activities, have impaired quality of life, and frequently are disabled.




1 American Chronic Pain Association (www.theacpa.org, 2019)
2 Vincent A, Lahr BD, Wolfe F, Clauw DJ, Whipple MO, Oh TH, Barton DL, St Sauver J. Prevalence of fibromyalgia: a population-based study in Olmsted County, Minnesota, utilizing the Rochester Epidemiology Project. Arthritis Care Res (Hoboken). 2013;65(5):786-92.
3 Robinson RL. Kroenke K, Mease P, Williams DA, Chen, Y, D’Souza D, Wohlreich, M, McCarberg, B. Burden of illness and treatment patters for patients with fibromyalgia. Pain Medicne, 2012; 13:1366-1376.
Long COVID
Long COVID or Post-Acute Sequelae of COVID-19 (PASC), is a condition that survivors of COVID-19 infection experience at varying degrees. It is a chronic disabling condition that is expected to result in a significant global health and economic burden.1 The symptoms include intense fatigue, fevers, sleep problems, pain, and cognitive issues (“brain fog”). Post infection, many patients experience one or many of the symptoms of Long COVID: some patients have initial symptoms that become prolonged; others manifest entirely new syndromes that impact more than one system or organ. According to a recent publication in the Journal of American Medical Association (JAMA), over 1 in 10 healthcare workers who had recovered from COVID-19 were still coping with at least one moderate to severe symptom eight months later.2 Studies have reported that persistence of symptoms following SARS-CoV-2 infection occurs in more than 13% of patients.3 There is currently no approved drug for the treatment of Long COVID.
1 Briggs, Andrew, and Anna Vassall. “Count the cost of disability caused by COVID-19.” (2021): 502-505.
2 Symptoms and functional impairment assessed 8 Months after mild COVID-19 among health care workers. Havervall S, Rosell A, Phillipson M, Mangsbo SM, Nilsson P, Hober S, Thålin C. JAMA. 2021 Apr 7.
3September 1, 2022- CDC – https://www.cdc.gov/coronavirus/2019-ncov/long-term-effects/index.html


Cocaine Intoxication
Cocaine is an illegal recreational drug which is taken for its pleasurable effects and associated euphoria. Pharmacologically, cocaine blocks the reuptake of the neurotransmitter dopamine from central nervous system synapses, resulting in the accumulation of dopamine within the synapse and an amplification of dopamine signaling and its role in creating positive feeling. With the continued use of cocaine, however, intense cocaine cravings occur resulting in a high potential for abuse and addiction (dependence), as well as the risk of cocaine intoxication. Cocaine intoxication refers to the deleterious effects on other parts of the body, especially those involving the cardiovascular system. Common symptoms of cocaine intoxication include tachyarrhythmias and elevated blood pressure, either of which can be life-threatening. As a result, individuals with known or suspected cocaine intoxication are sent immediately to the emergency department, preferably by ambulance in case cardiac arrest occurs during transit. There are approximately 505,000 emergency room visits for cocaine abuse each year in the U.S., of which 61,000 require detoxification services.
According to the National Institute on Drug Abuse, about 16,000 individuals died of cocaine overdose in 2019.1 According to a recent report by the U.S. Centers for Disease Control and Prevention2, and covered by news reports3,4, among all 2017 U.S. drug overdose deaths, approximately 20% involved cocaine. Overdose deaths involving cocaine increased 34 percent from 2016 to 2017.
1 Overdose Death Rates — National Institute on Drug Abuse — https://www.drugabuse.gov/related-topics/trends-statistics/overdose-death-rates
2 Kariisa, M, Scholl, L, Wilson, N, Seth, P, Hoots, B. Drug Overdose Deaths Involving Cocaine and Psychostimulants with Abuse Potential — United States, 2003–2017. MMWR Weekly / May 3, 2019 / 68(17);388–395 — https://www.cdc.gov/mmwr/volumes/68/wr/mm6817a3.htm?s_cid=mm6817a3_w; accessed May 11, 2019
3 Fottrell, Q. MarketWatch, Fatal drug overdoses involving cocaine and other stimulants have surged by over 52%8, May 3, 2019 — https://www.marketwatch.com/story/fatal-drug-overdoses-involving-cocaine-and-other-stimulants-have-surged-by-over-52-2019-05-03; accessed May 11, 2019
4 Cocaine deaths up in U.S. and opioids are a big part of it. Associated Press. https://www.msn.com/en-us/news/us/cocaine-deaths-up-in-us-and-opioids-are-a-big-part-of-it/ar-AAAOxs8?ocid=se; accessed May 11, 2019
Migraine
Migraine is a neurological condition that manifests in throbbing headache, often on one side of the head, that lasts at least four hours. It can also be accompanied by nausea, vomiting, visual disturbances, and sensitivity to bright light, strong smells, and loud noises1. Epidemiological studies indicate that globally, approximately 1.2 billion individuals suffer from migraines annually.2 In the U.S., approximately 39 million Americans suffer from migraines and among these individuals, approximately four million experience chronic migraines (15 or more headache days per month).2




Agitation in Alzheimer’s Disease
Agitation in Alzheimer’s disease (AAD) is a common behavioral symptom experienced by a majority of patients with Alzheimer’s Disease. AAD, which includes emotional lability, restlessness, irritability, and agitation,1 is one of the most distressing and debilitating of the behavioral complications of Alzheimer’s disease. Both sleep disturbances and agitation are common and co-morbid features of Alzheimer’s disease.1,2,3 It is associated with significant negative consequences for both patients as well as their caregivers. Development of agitation, or its worsening, is one of the most common reasons for patients having to transition to nursing homes and other long-term care settings.
To date, there are no FDA approved treatment for behavioral symptoms such as agitation and aggression which affects the quality of life of both the patients and caregivers1.
Agitation is likely to affect more than half of the 5.3 million Americans who currently suffer from Alzheimer’s disease, and this number is expected to nearly triple by 2050.4 The presence of agitation nearly doubles the cost of caring for patients with Alzheimer’s disease, and agitation is estimated to account for more than 12 percent of the $256 billion in healthcare and societal cost of associated with Alzheimer’s disease for the year 2017 in the United States. 4
AAD is recognized by the FDA as a serious condition with an unmet medical need.
1 Canevelli M, Valletta M, Trebbastoni A, Sarli G, D’Antonio F, Tariciotti L, de Lena C, Bruno G. Sundowning in Dementia: Clinical Relevance, Pathophysiological Determinants, and Therapeutic Approaches. Front Med (Lausanne). 2016;3:73.
2 Rose K, Specht J, Forch W. Correlates among nocturnal agitation, sleep, and urinary incontinence in dementia. Am J Alzheimers Dis Other Demen. 2015;30(1):78-84.
3 Shih YH, Pai MC, Huang YC, Wang JJ. Sundown Syndrome, Sleep Quality, and Walking Among Community-Dwelling People With Alzheimer Disease. J Am Med Dir Assoc. 2017;18(5):396-401.
4 The Alzheimer’s Association. Alzheimer’s Disease Facts and Figures. https://www.alz.org/alzheimers-dementia/facts-figures.


Alcohol Use Disorder
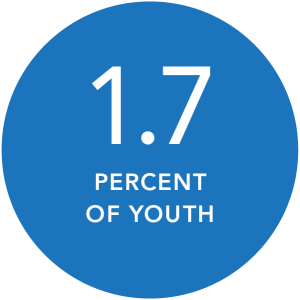
Alcohol use disorder (AUD) is a medical condition characterized by an impaired ability to stop or control alcohol use despite adverse social, occupational, or health consequences. It encompasses the conditions that some people refer to as alcohol abuse, alcohol dependence, alcohol addiction, and the colloquial term, alcoholism. Considered a brain disorder, AUD can be mild, moderate, or severe. Lasting changes in the brain caused by alcohol misuse perpetuate AUD and make individuals vulnerable to relapse. According to a national survey, 14.1 million U.S. adults ages 18 and older1(5.6 percent of this age group2) had AUD in 2019. Among youth, an estimated 414,000 adolescents ages 12–171 (1.7 percent of this age group2) had AUD during this timeframe.